Cataracts, commonly referred to as “cloudy eye” by some, are a condition characterized by the clouding or whitening of the eye’s lens, leading to significant vision loss. Typically associated with aging, cataracts develop gradually and are more prevalent in individuals aged 60 and above. Symptoms include blurred vision, sensitivity to light, and difficulty seeing in low-light conditions. Cataracts progress through stages, starting with minor visual disturbances in the early stage, advancing to significant impairment in the later stages. Treatment involves surgical removal of the cloudy lens and replacement with an artificial one, restoring clear vision.
What is Cataract?
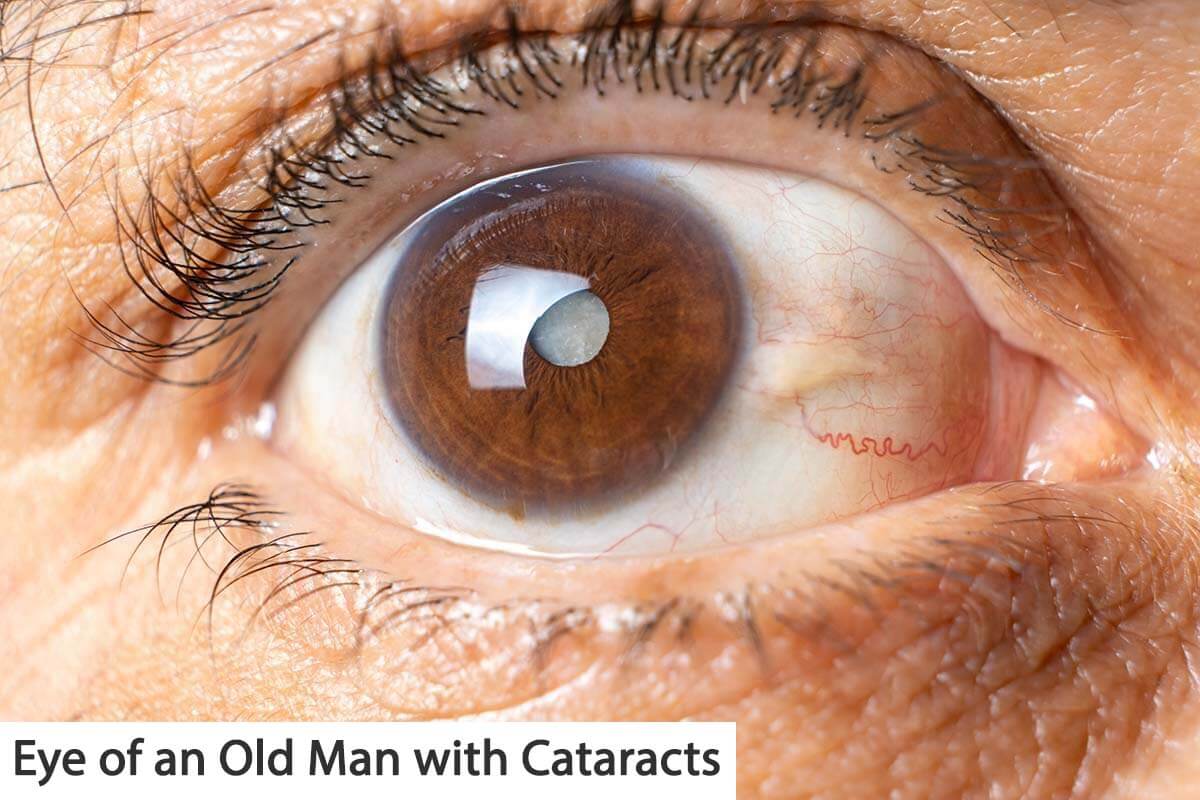
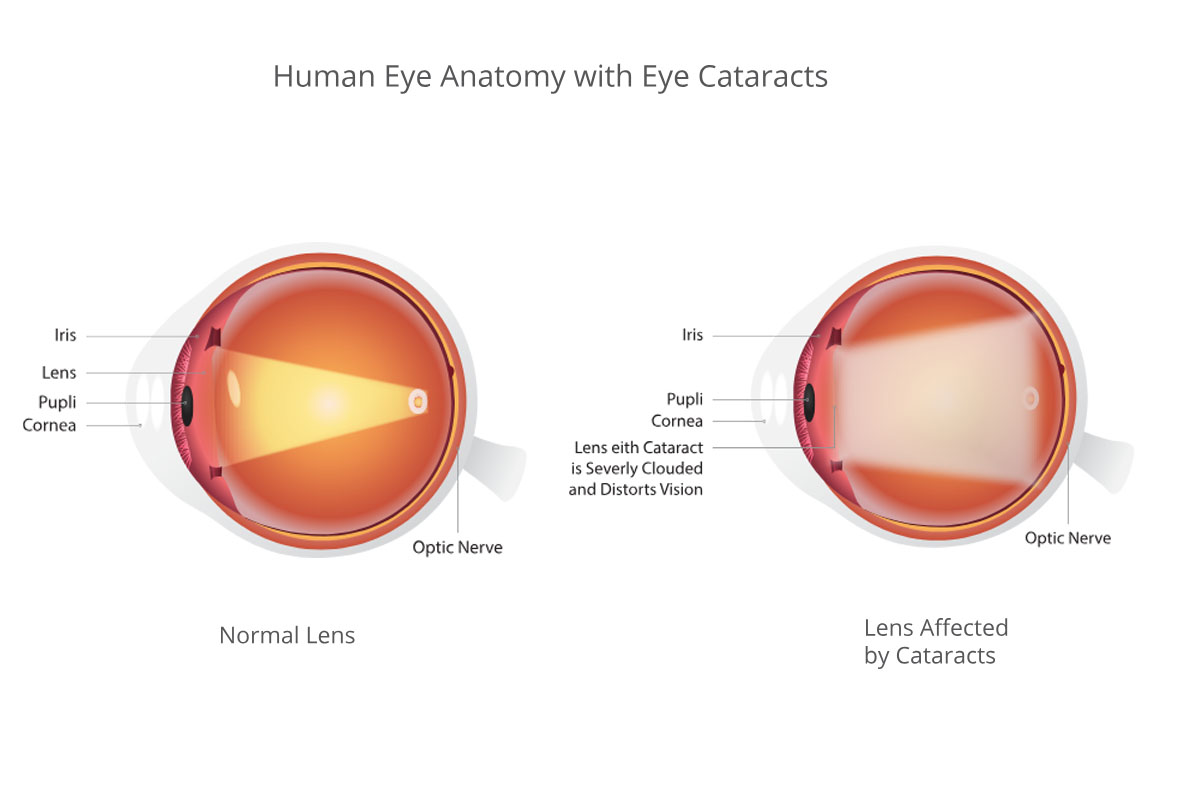
Cataracts are a prevalent eye condition characterized by the loss of transparency in the eye’s lens, leading to impaired vision. More specifically, they manifest as brown or yellow discolorations within the lens, accompanied by blurry areas that gradually decrease visual acuity.
Comprehensive Overview of Cataract Subtypes, Stages, and Progression
Cataracts encompass various subtypes, each with distinct characteristics and underlying causes. These subtypes include congenital cataracts, which occur rarely and pose higher surgical risks due to their presence from birth. Traumatic cataracts stem from eye injuries or accidents, while the most prevalent form, senile cataracts, develops with age. Understanding these subtypes is crucial for appropriate diagnosis and management strategies.
Cataracts exhibit diverse subtypes and stages, each characterized by distinct features and implications for vision. Subtypes include nuclear, cortical, corticonuclear, and posterior subcapsular cataracts, delineated by the location of lens opacity. Posterior subcapsular cataracts, often termed cortisone cataracts, are notably associated with corticosteroid usage, while congenital posterior polar cataracts result from innate damage to the lens capsule. Diabetic patients may present with snowflake cataracts, a unique manifestation.
Stages of cataracts are classified based on hardness and progression, directly correlating with declining vision.
Stage 1: Minimal loss of lens transparency with slight impact on vision.
Stage 2: Significant reduction in lens transparency, resulting in vision decline below 50%, sometimes accompanied by rapid changes in glasses prescription.
Stage 3: Pronounced opacity or discoloration of the lens, leading to vision decrease to 10% or lower.
Stage 4: Complete opacity of the lens, rendering vision extremely limited—often restricted to perceiving light or close hand movements without discerning details.
Following Stage 4, cataracts may enter the intumescent phase, marked by lens swelling and increased intraocular pressure. This phase poses further risks, including potential lens protein release and subsequent elevation of intraocular pressure. Understanding these subtypes, stages, and progression dynamics is vital for effective diagnosis, management, and intervention in cataract patients.
Symptoms of Cataracts
Cataracts manifest through various symptoms that affect vision and daily activities. These symptoms include:
Light Scattering: Increased sensitivity to light or glare, particularly in bright environments.
Decreased Distance Vision: Difficulty seeing objects clearly at a distance, resulting in blurred vision.
Change in Glasses Prescription: Regular changes in eyeglass or contact lens prescriptions due to fluctuating vision.
Feeling of Looking Through Frosted Glass: Visual disturbances akin to looking through frosted or cloudy glass.
Near Vision Changes: In nuclear type cataracts, stages 1 and 2 may temporarily improve near vision, but as cataracts progress to stage 3, near vision may deteriorate.
Severe Vision Impairment: Stage 4 cataracts cause a drastic decrease in vision, often falling below 1%.
Recognizing these symptoms is crucial for timely diagnosis and appropriate management of cataracts. Individuals experiencing any of these symptoms should seek evaluation by an eye care professional for proper assessment and treatment options.
Causes of Cataracts
Cataracts arise from various underlying factors, each contributing to the development of this common eye condition.
Trauma: Traumatic cataracts stem from damage to the lens capsule and supporting ligaments due to physical injury or trauma to the eye.
Congenital Disorders: Congenital cataracts result from developmental abnormalities in the fetus during pregnancy, leading to lens malformations.
Diabetic Snowflake Cataracts: Fluctuations in blood sugar levels in diabetic patients can cause the formation of distinctive snowflake cataracts.
Environmental Factors: Prolonged exposure to ultraviolet (UV) rays and smoking are recognized risk factors for cataracts, contributing to their development over time.
In age-related cataracts, the most prevalent form, a multifactorial mechanism is at play:
Nuclear Sclerosis: Aging leads to compression and hardening of the central lens material, known as the nucleus, contributing to nuclear sclerosis.
Protein Changes: Abnormal chemical and structural alterations occur in the proteins of the lens with advancing age, affecting transparency and function.
Pigmentation: Accumulation of proteins in the lens results in the formation of yellow and brown pigments, further contributing to cataract development.
Ionic Changes: Age-related changes in the ionic composition of the lens contribute to its deterioration and opacity over time.
Understanding these diverse causes of cataracts is essential for effective prevention, early detection, and management strategies tailored to individual patients
Demographics of Cataracts
Cataracts affect individuals across various demographics, with age serving as the predominant factor in their onset. Typically emerging after the age of 55, the incidence of age-related senile cataracts escalates with advancing years, with prevalence rates notably increasing among older age groups. Trauma, diabetes, corticosteroid usage, and, albeit rarely, congenital factors also contribute to cataract development.
Eye injuries or accidents can precipitate cataracts regardless of age, while diabetic individuals face heightened risks due to fluctuating blood sugar levels. Prolonged cortisone or corticosteroid use elevates susceptibility, and although rare, congenital cataracts may occur in newborns due to prenatal developmental anomalies. Understanding these demographic nuances is pivotal for targeted prevention and intervention strategies aimed at mitigating cataract progression and associated vision impairment.
Does Cataract Cause Blindness?
Cataracts represent one of the most prevalent and treatable causes of blindness globally. While stage 4 cataracts can diminish vision to levels approaching blindness, vision typically improves following surgical intervention. However, in cases where stage 4 cataracts persist without surgical correction for an extended period, there is a risk of lens protein melting, leading to a dangerous increase in intraocular pressure. This scenario can result in irreversible blindness if left untreated. Hence, timely diagnosis and appropriate cataract surgery are crucial for preventing blindness and restoring vision effectively.
What Should Be Done to Prevent Cataracts?
To prevent cataracts, proactive measures are essential, beginning with safeguarding against harmful UV rays from the sun, starting in childhood. Utilizing hats and sunglasses effectively shields the eyes from UV radiation, minimizing the risk of cataract formation. Additionally, prudent management involves avoiding unnecessary cortisone use and maintaining vigilant monitoring of blood sugar levels among diabetic individuals, effectively curbing the escalation of cataract risk. These preventive actions, coupled with regular eye examinations, serve as critical steps in preserving eye health and mitigating the onset of cataracts.
Diagnosis of Cataracts
Diagnosing cataracts typically involves a combination of visual acuity testing and biomicroscopic eye examination. During these evaluations, an eye care professional assesses visual clarity and examines the eye’s structures using specialized instruments. In certain instances, additional diagnostic procedures such as eye examination with dilating eye drops may be necessary to confirm the presence of cataracts and evaluate their severity. This comprehensive approach ensures accurate diagnosis and enables healthcare providers to tailor treatment plans effectively for individuals affected by cataracts.
Perceiving the Environment with Cataracts: Visual Impairment and Symptoms
Individuals with cataracts experience various visual disturbances that affect their perception of the surrounding environment. The entire visual field is impacted, resulting in symptoms such as blurred or hazy vision, akin to viewing the world through frosted glass. Posterior subcapsular cataracts, in particular, can exacerbate light scattering and glare. Initially, early-stage cataracts may paradoxically improve near vision while worsening distance vision. However, as cataracts progress, both near and distance vision deteriorate significantly. In advanced stages, characterized by end-stage cataracts, vision diminishes to below 1%, severely impairing daily activities and quality of life. Understanding these visual manifestations is crucial for timely diagnosis and intervention to mitigate the impact of cataracts on visual function.
Cataract Treatment: Surgical Intervention for Vision Restoration
The primary treatment for cataracts involves surgical removal of the affected lens followed by the insertion of an artificial lens to restore vision. Cataract surgery is a safe and effective procedure aimed at improving visual clarity and quality of life for affected individuals.
Are There Alternative Cataract Treatment Options?
Cataracts are primarily treated through surgical removal of the affected lens, which is replaced with an artificial lens to restore vision. Cataract surgery typically lasts around 15-20 minutes and is known for its efficacy and safety.
Potential Complications Post-Cataract Surgery
Cataracts typically do not recur after surgical treatment, but a potential complication may arise with the capsule behind the implanted lens. Over time, this capsule may develop opacities, causing visual disturbances. However, such instances can be effectively managed through a procedure known as YAG Laser Capsulotomy. Conducted as an outpatient procedure, YAG Laser Capsulotomy takes approximately 5 minutes and efficiently resolves the whitening of the capsule, restoring clear vision. This approach ensures ongoing visual health and quality of life for individuals who have undergone cataract surgery.